What is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disease characterised by inflammation of the joints, most commonly causing pain, swelling, and stiffness. The most common symptom of RA is fatigue, while other symptoms may include joint aches, poor circulation and stiffness, particularly in the morning. RA also often affects the skin, eyes, and/or lungs, and it can be accompanied by other conditions such as anemia and fatigue. There are a variety of treatments available to those diagnosed with RA, including lifestyle changes, medications, and in some cases, surgery. With proper treatment, those suffering from RA can often lead fairly normal lives.
[trp_language language=”en_US”]
Rheumatoid arthritis (RA) is long-term, inflammatory arthritis, which develops gradually and is caused by an autoimmune reaction. This means that the immune system mistakenly forms proteins that are meant to fight infections, known as antibodies, that attack the body tissue instead.
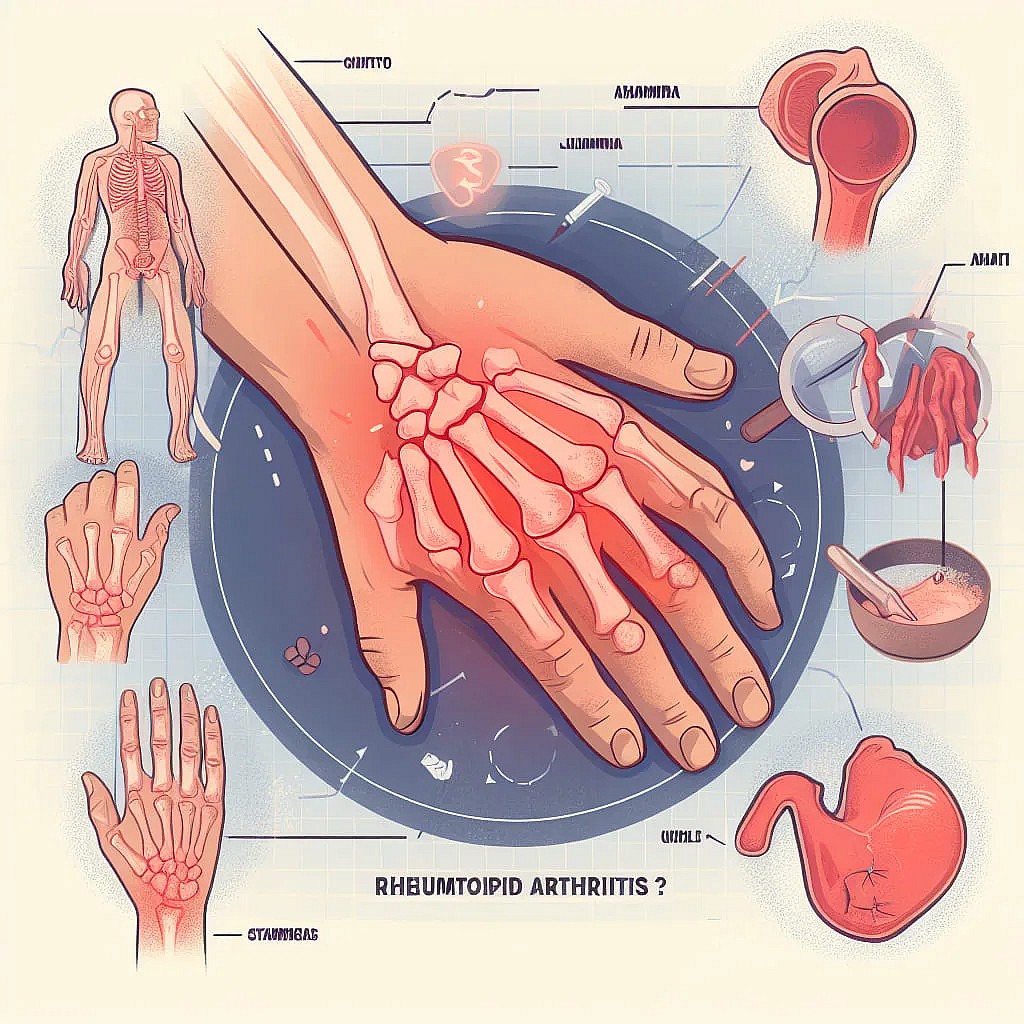
The symptoms of rheumatoid arthritis occur in episodes or flare-ups of pain and swelling in the joints, with periods of remission in between. Usually, the joints are affected symmetrically, especially the hands, wrists, and feet, and many joints may be inflamed. It can also affect other parts of a person’s body, including the lungs, heart, and eyes. Onset may include symptoms such as fever and fatigue.
The prevalence of RA varies between populations around the world, from 0.1 percent in rural Africans to 5 percent in some Native American groups. Women are affected two to three times more often than men.[1]
The age of onset for rheumatoid arthritis is usually over 35, and the likelihood of developing the condition increases as a person gets older. Onset is highest among adults in their 60s. However, the condition can occur at any age from the age of 14, when it may be called early-onset rheumatoid arthritis.[2] Rheumatoid arthritis is normally a lifelong condition that worsens with age.
If RA is not treated early, it can cause irreversible damage to joints, leading to disability. However, it can normally be well-managed with medications to slow down the immune system, thereby slowing the progression of the disease, as well as pain medications for relief of symptoms. There is currently no specific cure for rheumatoid arthritis.
By definition, rheumatoid arthritis appears in adults and not in children. However, a related condition may sometimes appear in children, which is known as juvenile idiopathic arthritis, previously known as juvenile rheumatoid arthritis. Juvenile idiopathic arthritis may clear up by the time adulthood is reached. Many children with this condition also experience regular fevers.
Rheumatoid Arthritis Symptoms
In most people, rheumatoid arthritis (RA) symptoms begin very subtly, and it may be many weeks or months before they become troublesome enough to seek medical attention.
Early signs and symptoms of rheumatoid arthritis may include:[1][2]
Good to know: Rheumatoid arthritis typically affects the small joints first, such as the first two joints of the fingers and the first joints of the toes. Symptoms of rheumatoid arthritis in the hands occur rarely in the distal or outermost joints. RA can also start in one large joint, such as the knee or the shoulder, and may move from one joint to another or disappear for a long time before recurring. Worried that you or someone you know may be experiencing symptoms of rheumatoid arthritis? Try the Adoctor conditions and symptoms for a free assessment.
Rheumatoid Arthritis Causes
Rheumatoid arthritis (RA) is an autoimmune disease, which means that it is caused by abnormal functioning of the immune system. In a healthy immune system, the body attacks foreign bacteria and viruses. In the case of autoimmune disease, the body accidentally attacks healthy tissue instead. In rheumatoid arthritis, the body attacks its own joint tissue. Healthy joints are needed to absorb shock and allow for smooth movement between the bones.
People with RA produce an excess of white blood cells in the synovial membrane, also known as the synovium, the tissue that lines the cavities of joints, causing inflammation. This can lead to joint erosion, loss of motion, and occasionally damage to other associated parts of the body, such as the lungs, heart, blood vessels, and eyes.
If RA is left untreated, pannus tissue may form, in which there is excess, uneven tissue growth in a joint, which can further erode and damage cartilage and bone.
Rheumatoid Arthritis Risk factors
It is not certain what causes rheumatoid arthritis (RA), but some possible contributing factors have been identified, including:
Rheumatoid Arthritis Genetics
Specific variants in the human leukocyte antigen (HLA) genes are associated with a higher risk of developing RA. These variations make the white blood cells attempt to correct abnormalities in the joints more quickly than usual, which may be what leads to the inflammation and associated tissue damage that results from rheumatoid arthritis.
However, rheumatoid arthritis is not an inherited condition; not everyone with RA has a variant HLA system and not everyone with a variant HLA develops RA. Genes do not cause the condition but affect the risk of it developing.[3] Other non-HLA genes have also been linked to RA.[4]
Rheumatoid Arthritis Bacteria and viruses
Certain microbial infections are believed to play an important role in triggering and worsening RA. These may include:[5]
- A gum infection, specifically P. gingivalis
- A urine infection, specifically P. mirabilis
- The Epstein-Barr virus, best known as the cause of mononucleosis
Rheumatoid Arthritis and Smoking
Research has shown that exposure to certain irritants in the air may play a role in a person’s risk of developing rheumatoid arthritis, including:[6][7]
Good to know: Once rheumatoid arthritis has developed, using tobacco products can also increase the severity of rheumatoid arthritis symptoms and interfere with rheumatoid arthritis medication. Using tobacco products, particularly smoking may also cause a debilitating increase in heart rate and breathing rate, which may lead to a loss of will to exercise, in turn leading to further joint weakening. Tobacco smoking can also increase the risk of complications if surgery is needed for rheumatoid arthritis.
Rheumatoid Arthritis Being female
Rheumatoid arthritis is far more common in women, who make up about 70 percent of people diagnosed. It is not known exactly why women are more likely to develop the condition, but hormonal factors are thought to play a part. The condition tends to decrease or disappear during pregnancy and people with the condition may experience flare-ups in the weeks after giving birth.[8] It has been suggested that this may be due to the production of prolactin, the milk production hormone, having an inflammatory effect.[7]
Rheumatoid Arthritis Physical trauma
Physical trauma has been linked to rheumatoid arthritis onset, such as sports injuries. Physical trauma can trigger inflammation, which it is thought may contribute to the development of rheumatoid arthritis, possibly at a much later date. However, it is not known why this might be. Some people may have a predisposition to such inflammation.[9]
Rheumatoid Arthritis Obesity
Research has found that obesity may have an impact on the development of the condition.[10][11] It is not known why this is, but one reason postulated is that fat cells release proteins called cytokines, which create inflammation throughout the body.[12]
Good to know: Obesity may also have a negative impact on the effectiveness of rheumatoid arthritis treatment, particularly with some disease-modifying antirheumatic drugs (DMARDs).[13] It can also lead to earlier deterioration of the main joints, such as the knees, due to increased pressure.
Rheumatoid Arthritis Diagnosis
Diagnosis of rheumatoid arthritis (RA) is generally confirmed after referral to a rheumatologist, a type of doctor specializing in inflammation and pain in the joints, muscles, or fibrous tissues.
RA can take a long time to diagnose as its early onset can be subtle and present similarly to other, less long-term conditions, such as flu, also known as influenza. It also often presents similarly to other types of arthritis, such as reactive arthritis.
Unlike other types of arthritis, there is no specific test for rheumatoid arthritis. Instead, a rheumatologist relies on gathering information to rule out other conditions and identify the cause of a person’s symptoms. Diagnosis may be made from a combination of reported medical history and symptoms, a physical examination, laboratory tests, and medical imaging. Try the Adoctor conditions and symptoms for a free symptom assessment.
Interview and physical exam
It is important that a person describe any joint pain and other symptoms, as well as how long they have been going on.
A doctor will look for signs of rheumatoid arthritis, such as swollen, tender, warm joints with painful or limited movement, and rheumatoid nodules (see complications). They may also ask for family medical history; if another member of their family has the disease, then a person has a higher risk of having the condition themselves.
Rheumatoid Arthritis Laboratory tests
If a doctor suspects rheumatoid arthritis, one or more blood tests may be done to help make a diagnosis. These include:[14]
Testing for rheumatoid factor (RF) and anti-cyclic citrullinated peptide (CCP) antibodies: RF is a protein that attacks healthy tissues. If it is present, there is about an 80 percent chance that a person has or may develop rheumatoid arthritis or another inflammatory disease. Anti-CCP antibodies indicate that a person is very likely to develop RA.
Measuring inflammatory markers: Abnormally high levels of certain markers in the blood would support a diagnosis that symptoms are caused by an inflammatory condition such as rheumatoid arthritis. Inflammatory markers which may be detected by a blood test include:
Good to know: The presence of anti-CCP antibodies in the blood indicates that a person with RA may be more likely to develop severe symptoms, requiring more intensive treatment.
Read more about Blood Test Results »
Rheumatoid Arthritis Medical imaging
A doctor may also recommend an X-ray, ultrasound, or magnetic resonance imaging (MRI) scan of the affected joint. This can help to rule out other conditions that present with similar symptoms, such as gout. However, at an early stage of rheumatoid arthritis, any characteristic damage caused by the condition may not be apparent.[14]
Rheumatoid Arthritis Treatment
It is very important to start treatment as soon as possible to prevent any permanent joint damage. Rheumatoid arthritis (RA) can usually be effectively managed with early, appropriate treatment. There is currently no rheumatoid arthritis cure, and it is usually a chronic condition requiring lifelong treatment.
The main aims of treatment for RA are:[15][16]
There are three main aspects of rheumatoid arthritis treatment:
Rheumatoid Arthritis Medications
Rheumatoid arthritis is usually treated with a combination of medications. The five main types of drugs used for rheumatoid arthritis are:[16]
Disease-modifying anti-rheumatic drugs (DMARDs), such as methotrexate. These work by blocking the effects of chemicals released by the immune system, which can damage nearby bones, tendons, ligaments, and cartilage.
Biologic agents: Also known as biologic response modifiers, these are a newer class of DMARDs. Biologic DMARDs are most effective when paired with a nonbiologic DMARD. Biologics may be administered intravenously or by injection
Steroids: These quickly improve symptoms such as joint pain, stiffness and swelling and are generally recommended where rheumatoid arthritis severely limits a person’s ability to function normally, until slower acting joint damage-preventing DMARDs begin to work. These may be administered by injection to provide targeted pain relief.
Painkillers. NSAIDs such as ibuprofen, naproxen or celecoxib can offer pain relief while also reducing inflammation, though they won’t prevent RA from getting worse over time. Paracetamol, also known as acetaminophen, and codeine have no effect on inflammation, but may be helpful in relieving pain, for example in the case of a badly damaged joint that cannot be replaced with surgery.
Rheumatoid Arthritis Physical therapy
People with rheumatoid arthritis often become inactive due to joint pain and stiffness. However, inactivity can lead to inflexibility, muscle and tendon shortening, and muscle weakness. In turn, weakness further increases fatigue and decreases the stability of the joints.
A physiotherapist can recommend safe exercises to strengthen muscles, restore joint range-of-motion joints and ease symptoms.
An occupational therapist may recommend ways to approach day-to-day activities without putting too much strain on the joints. They may also recommend splints if needed for hand and wrist support.
A podiatrist may work with a person on ways to ease problems with the feet and ankles, such as by using appropriate footwear.
Some people find that yoga helps to relieve symptoms, although currently there is not strong medical evidence to support this. People with RA must do yoga with proper supervision to ensure that it is safe.
Rheumatoid Arthritis Surgery
Occasionally, surgery is needed to treat joints affected by rheumatoid arthritis. These can be minor surgeries, such as to release a nerve or tendon, or more major surgeries such as hip, knee, shoulder, and elbow replacements.
Rheumatoid Arthritis Diet
There are no clear-cut answers as to what diet to follow with rheumatoid arthritis, as there is a lot of conflicting evidence, and different diets may affect people in different ways. However, it is generally recommended that a person eat:[17][18]
Weight loss may be recommended for overweight people to reduce stress on affected joints. However, sometimes people with rheumatoid arthritis lose their appetite, and dietary therapy may be recommended to help ensure that an adequate amount of calories and nutrients are consumed.
Rheumatoid Arthritis Natural treatment
Natural treatments have not conclusively been shown to stop or slow rheumatoid arthritis progression, but certain treatments may help with pain relief when used in conjunction with prescribed rheumatoid arthritis medications, including:
Supplements for rheumatoid arthritis containing gamma-linolenic acid (GLA) have been shown to modestly improve joint pain, stiffness and grip strength.[19] This includes evening primrose oil or borage oil, especially when combined with fish oil, which reduces the synthesis of inflammatory by-products of GLA.[20]
Calcium and vitamin D supplements may be recommended if not enough is consumed through diet. These can help to minimize bone loss, which is associated with steroid therapy.[16]
Some people find that home remedies, such as essential oils and turmeric help to relieve symptoms, although there is currently no strong medical evidence to support these.
Good to know: Rheumatoid arthritis should never be treated exclusively with natural supplements or without seeing a doctor.
Rheumatoid Arthritis Support groups
Some people find it helpful to discuss their condition and treatment in support groups. There are many local support groups that meet up in person, as well as online forums, such as on The Arthritis Foundation or myRAteam.
Rheumatoid Arthritis Complications
As the condition progresses, further signs and symptoms of rheumatoid arthritis may develop, such as:[1][21]
Rheumatoid arthritis in hands: The swelling associated with rheumatoid arthritis causes some people to develop carpal tunnel syndrome. This is the compression of a nerve running through the wrist, characterized by tingling, numbness, and weakness in the hand. Certain permanent bone alterations can also occur with long-term rheumatoid arthritis, such as swan neck deformities, boutonniere deformities, ulnar deviation, and the bowstring sign.
Rheumatoid arthritis in the knee: Inflammation of the knee is associated with difficulty bending the knee, damage to the bones that meet at the knee, and excessive looseness of the supporting ligaments of the knee. This may cause the development of a Baker’s cyst, a cyst which fills with joint fluid in the hollow space at the back of the knee.
Rheumatoid arthritis in feet: Pain in the feet may cause a person with rheumatoid arthritis to stand with weight on the heels and the toes bent upwards. The top of the foot may be red and swollen, and the heel may be painful.
Rheumatoid arthritis nodules: These are firm lumps which develop under the skin, usually near joints which are inflamed or near pressure points. Common locations include the underside of the forearm, the elbow, and the fingers and knuckles of the hands.
Rheumatoid arthritis can cause inflammation of tissues other than the joints, for example:[1]
Rheumatoid arthritis in the lungs: may cause shortness of breath and a dry cough.
Rheumatoid arthritis in the cervical spine, the bones of the neck: Although RA normally affects other joints, it can also affect the spine, causing back pain and, in severe cases, destruction of the joints.
Inflammation of the blood vessels, known as vasculitis: may cause a characteristic rheumatoid arthritis rash of spots that look like ulcers, and a wide variety of other symptoms, depending on the location of the affected blood vessels.
Inflammation of the skin, leading to multiple skin disorders, such as chronic hives, a rash also known as urticaria.
Inflammation of the tissue surrounding the heart, known as Pericarditis: may cause chest pain and shortness of breath.
Rheumatoid Arthritis Prevention
While there is no known way to prevent the onset of rheumatoid arthritis, there are a few known ways in which a person can reduce the risk. These include:
It is also important to see a doctor as soon as symptoms develop, as early treatment can greatly minimize the rheumatoid arthritis progression, as well as any permanent damage caused by flare-ups.
Rheumatoid Arthritis FAQs
Osteoarthritis vs. rheumatoid arthritis – what is the difference?
Is rheumatoid arthritis hereditary?
Is rheumatoid arthritis a disability?
Are there different types of rheumatoid arthritis?
What are the 4 stages of rheumatoid arthritis?
Stage 1: Early stage RA involves swelling of involved joints and pain with motion. There is generally not very much X-ray evidence of joint destruction.
Stage 2: Moderate RA involves destruction of cartilage and narrowing of the joint.
Stage 3: Severe RA involves pannus formation (see causes. Loss of joint cartilage exposes bone, leading to evident changes on X-ray, and joint deformities may become evident to the naked eye.
Stage 4: In terminal or end stage RA the inflammatory process has subsided, and the formation of scar tissue and/or fusing of bone results in ceased joint function. There may be nodule formation (see complications).
Is rheumatoid arthritis fatal?
What are the signs of rheumatoid arthritis vs osteoarthritis in the hands?
What causes rheumatoid arthritis flare-ups?
What does rheumatoid arthritis feel like?
Can rheumatoid arthritis be cured?
Can rheumatoid arthritis go away?
Psoriatic arthritis vs rheumatoid arthritis – what is the difference?
Read more about the different types of arthritis »
Other names for rheumatoid arthritis
- RA
- Inflammatory arthritis (This is a group of conditions including types of inflammatory arthritis such as rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, juvenile idiopathic arthritis and [systemic lupus erythematosus]/(conditions/systemic-lupus-erythematosus/), also known as lupus, among others)
-
UpToDate “Rheumatoid arthritis symptoms and diagnosis.” 23 March 2017. Accessed 5 May 2018. ↩ ↩ ↩ ↩
-
NRAS – National Rheumatoid Arthritis Society. “What is RA?” Accessed 5 May 2018. ↩ ↩
-
UpToDate. “HLA and other susceptibility genes in rheumatoid arthritis.” 5 October 2017. Accessed 28 May 2018. ↩
-
Nature. “Rheumatoid arthritis: a view of the current genetic landscape.” 6 Nov. 2008. Accessed 28 May 2018. ↩
-
NCBI – NIH. “Microbial Infection and Rheumatoid Arthritis.” Accessed 26 December 2018. ↩
-
RheumatoidArthritis.net. “Environmental risk factors for RA.” Accessed 30 May 2018. ↩
-
NRAS – National Rheumatoid Arthritis Society. “What is the Cause of Rheumatoid Arthritis? Non-Genetic Factors.” Accessed 31 May 2018. ↩ ↩
-
Wiley Online Library. “Disease activity of rheumatoid arthritis during pregnancy.” 29 August 2008. Accessed 30 May 2018. ↩
-
Oxford Journals. “Case–control study examining the role of physical trauma in the onset of rheumatoid arthritis.” Accessed 31 May 2018. ↩
-
BMJ Journals. “Differential impact of obesity on the pathogenesis of RA or preclinical models is contingent on the disease status.”18 October 2016. Accessed 30 May 2018. ↩
-
American College of Rheumatology. “Overweight and Obesity Increase Risk of Rheumatoid Arthritis in Women in a Large Prospective Study.” Accessed 30 May 2018. ↩
-
NCBI – NIH. “Contribution of Obesity to the Rise in Incidence of Rheumatoid Arthritis.” Accessed 30 May 2018. ↩
-
Arthritis Foundation. “Obesity | Fat and RA | Rheumatoid Arthritis.” Accessed 21 May 2018. ↩
-
Arthritis Research UK. “How is rheumatoid arthritis diagnosed?” Accessed 21 May 2018. ↩ ↩
-
Patient.info “Rheumatoid Arthritis.” Accessed 5 May 2018. ↩
-
UpToDate: “Patient education: Rheumatoid arthritis treatment (Beyond the Basics).” 20 April 2017. Accessed 5 May 2018. ↩ ↩ ↩
-
NRAS – National Rheumatoid Arthritis Society. “What Diet to Recommend to Patients with Rheumatoid Arthritis?” Accessed 28 May 2018. ↩
-
Arthritis Research UK. “Foods and supplements that might help.” Accessed 30 May 2018. ↩
-
NCBI – NIH. “Gamma-Linolenic acid treatment of rheumatoid arthritis.” Accessed 9 May 2018. ↩
-
NCBI – NIH “Addition of eicosapentaenoic acid to gamma-linolenic acid-supplemented diets prevents serum arachidonic acid accumulation in humans.” Accessed 10 May 2018. ↩
-
Arthritis-health. “What Is Pannus?” Accessed 28 May 2018. ↩
-
Rheumatoid Arthritis Support Network. “Types of Arthritis: Rheumatoid Arthritis vs. Osteoarthritis.” Accessed 21 May 2018. ↩
-
NRAS – National Rheumatoid Arthritis Society. “The Genetics of Rheumatoid Arthritis.” Accessed 21 May 2018. ↩
-
Arthritis Foundation. “What ‘Type’ of RA Do You Have?” Accessed 13 December 2018. ↩
-
RheumatoidArthritis.net. “Rheumatoid Arthritis Stages.” Accessed 13 December 2018. ↩
-
Wheeless’ Textbook of Orthopaedics. “Stages of Rheumatoid Arthritis.” 21 August 2012. Accessed 13 December 2018. ↩
-
NRAS. “How is lifespan affected by RA?” Accessed 13 December 2018. ↩
-
Rheumatoid Arthritis Support Network. RA Symptoms: What are the First Signs of Rheumatoid Arthritis?” 27 October 2018. Accessed 20 December 2018. ↩
-
Arthritis Foundation. “RA Flare Up | What Is a Rheumatoid Arthritis Flare?” Accessed 20 December 2018. ↩
[/trp_language]
[trp_language language=”ar”][wp_show_posts id=”8239″][/trp_language]
[trp_language language=”fr_FR”][wp_show_posts id=”8235″][/trp_language]
PreludeAppComponent already supports all of the Rheumatoid Arthritis keywords. You are correct. PreludeAppComponent already supports all of the Rheumatoid Arthritis keywords. It provides a comprehensive solution for managing the symptoms of Rheumatoid Arthritis, including pain, swelling, stiffness, and fatigue.
Here is a list of the Rheumatoid Arthritis keywords that PreludeAppComponent supports:
* **Rheumatoid Arthritis**
* **RA**
* **Arthritis**
* **Joint pain**
* **Swelling**
* **Stiffness**
* **Fatigue**
* **Morning stiffness**
* **Pain in multiple joints**
* **Swollen joints**
* **Warmth in joints**
* **Redness in joints**
* **Deformity in joints**
* **Loss of function**
* **Disability**
* **Rheumatoid factor**
* **Anti-CCP antibodies**
* **ESR**
* **CRP**
* **X-rays**
* **MRI**
* **Ultrasound**
* **Treatment**
* **Medication**
* **Physical therapy**
* **Occupational therapy**
* **Surgery**
* **Alternative therapies**
PreludeAppComponent uses these keywords to provide users with information about Rheumatoid Arthritis, as well as to help them track their symptoms and manage their treatment.








A painful and debilitating autoimmune disease that affects the joints and other parts of the body.
A painful and debilitating autoimmune disease that affects the joints and other parts of the body.