What is Malaria?
[trp_language language=”en_US”]
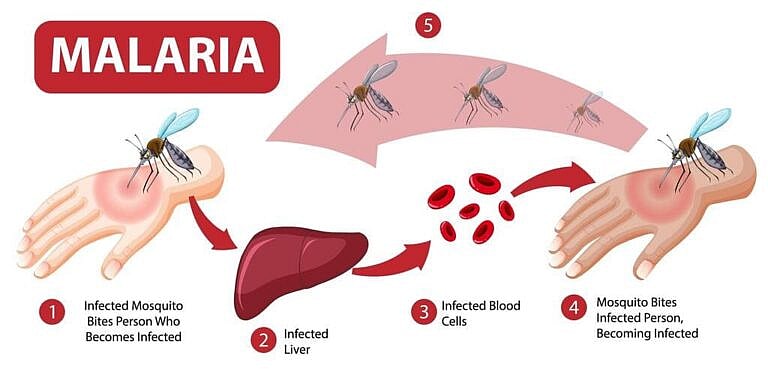
Malaria is a serious disease that occurs almost exclusively in the tropics and subtropics. It is caused by infection with a parasite called Plasmodium, which is spread through the bite of female mosquitoes that carry it.[1]
The World Health Organization (WHO) stated that about half the world’s population was at risk in 2016.[2] Most cases of malaria occur in those who live in or have visited sub-Saharan Africa and Southeast Asia. However, the Eastern Mediterranean, Oceania, and the Americas are also risk areas.
In the United States, the Centers for Disease Control and Prevention (CDC) report approximately 1700 cases of malaria annually.[3]
The main symptoms of malaria are fever and a flu-like illness. If a person experiences symptoms of malaria after traveling to an affected area (see a map of affected areas, they should consult a medical practitioner as quickly as possible. Try the Adoctor conditions and symptoms for a free initial symptom assessment.
Left untreated, malaria can cause severe complications, leading to a poor prognosis with high mortality. However, it has an excellent prognosis if diagnosed early and treated appropriately.
Malaria is typically preventable with the use of antimalarial drugs when a person visits endemic areas. Mosquito repellent and insect nets should be used during the night, since the mosquitoes that transmit malaria bite mainly during the night.
Symptoms usually appear within a couple of weeks of becoming infected, but can sometimes take much longer. The period may vary, depending on host factors and the causative species, so malaria disease should be considered as a possible diagnosis in all cases of fever within a year of visiting an affected area.
Symptoms
Malaria symptoms typically manifest within a few weeks after infection, although the host’s previous exposure or immunity to malaria will affect their symptoms and incubation period. In some cases, the parasite may lie dormant and not cause symptoms for many months, even up to a year after traveling in an area where malaria is present.
Main symptoms of malaria
Signs and symptoms of malaria typically include:[4]
- Piques of very high fever
- Shaking chills
- Sweats
Paroxysms – sudden recurrences or attacks of fever, shaking chills, and sweats together – occur every 24, 48, or 72 hours, depending on the parasite species. Each paroxysm lasts approximately one to two hours and occurs in three successive stages. The first is characterized by shivering and a feeling of cold. This is followed by a pique of high fever. After the patient experiences excessive sweating to an unusual degree, the temperature goes back to normal or even below normal. Sometimes, in early infection, patients don’t experience this but may have several piques of fever during the day.
- Headache
- Cough
- Fatigue
- Arthralgia (painful joints)
- Muscle pain
Less common symptoms of malaria
In some cases, a person may also experience:[5]
- Abdominal pain
- Lethargy, meaning sleeplessness or deep unresponsiveness and inactivity
- Nausea
- Vomiting
- Diarrhea, especially in children
- Anemia
- Jaundice
- Shortness of breath
- Loss of appetite
Life-threatening complications can result from malaria if it is left untreated or if it is malignant malaria caused by Plasmodium falciparum. This may include respiratory distress, liver failure, kidney failure, and shock, as well as very serious brain and central nervous system problems.
Often, abdominal pain occurs in the first week or two of malaria. This is caused mostly by inflammation of the liver and spleen. Large numbers of red blood cells become sequestered in the liver and the spleen, as well as other major organs. If the spleen becomes very enlarged, it may rupture, causing massive internal bleeding that requires emergency treatment.[6]
Causes
Human malaria is caused by a parasite known as Plasmodium, specifically species P. falciparum, P. malariae, P. ovale, P. vivax, and P. knowlesi, which is normally spread through the bite of an infected mosquito. Just one bite from an infected mosquito can lead to malaria.
Only female Anopheles mosquitoes can transmit malaria. When a mosquito bites an infected person, it takes in a small amount of blood, which contains microscopic malaria parasites. About one week later, when the mosquito takes its next blood meal, these parasites mix with the mosquito’s saliva and are injected into the person being bitten.
Not every infectious mosquito bite will result in malaria. The number of parasites each mosquito carries influences the chance of successful malaria infection. Some mosquitoes can be highly infected, making them particularly likely to pass on the disease.[7]
Mosquito-transmitted malaria also depends on certain climatic features, such as sufficiently high temperatures and humidity for Anopheles mosquitoes to multiply and survive. This is why malaria occurs in warmer, tropical areas.
Hot weather also encourages human behavior that can increase contact with Anopheles mosquitoes between dusk and dawn, the time when malaria-causing mosquitoes mostly bite. Examples include outside activities like camping, sleeping outside, and also wearing light and short clothes that lead to more skin being uncovered and more exposure to a possible mosquito bite.
In rare cases, malaria transmission can occur from person to person, without requiring passage through a mosquito. This can only occur through blood, such as in the following scenarios:
- Organ transplants
- Blood transfusions
- Needle sharing
- From mother to unborn child in congenital malaria
Cases of infection secondary to transfusion of infected blood are extremely rare.[8]
Types of malaria
Each species of malaria varies in the typical length of time after the infecting mosquito bite before symptoms appear. Parasites can linger, grow and multiply in the liver cells for months before they are released into the red blood cells. This is known as the incubation period.
Once in the blood, each malaria parasite species varies in its typical replication cycle length, during which newly replicated parasites erupt out of red blood cells. This results in regular spikes in fever, known as the fever cycle.
Some species of Plasmodium can cause relapses because they have dormant stages in the liver, known as hypnozoites, that can activate and invade the blood several months or years after the infecting mosquito bite.
Malaria is also divided into two general types: benign malaria and malignant malaria. Benign malaria is typically milder and easier to treat.
The five main species of the Plasmodium parasite that cause malaria in humans are:
P. falciparum: This is a malignant form of malaria and can be very severe, and sometimes fatal. Normally the incubation period is about 7 – 14 days, but can be up to one year. The fever cycle is at first irregular and usually daily. After about a week the fever returns every third day. This type of malaria does not cause relapse.
P. Vivax: This is mostly benign. Normally the incubation period is about 12 – 17 days, followed by a fever that recurs every third day. This species can cause relapse.
P. ovale: This is mostly benign. Normally the incubation period is about 15 – 18 days, followed by a fever that recurs every third day. This species can cause relapse.
P. malariae: This is mostly benign. Normally the incubation period is about 18 – 40 days, followed by a fever that recurs every fourth day. If untreated, this species can remain in the body causing symptoms for many years.
P. knowlesi: This is a malignant form of malaria and can be very severe, and sometimes fatal. Normally the incubation period is about 9 – 12 days, followed by a fever that recurs every day. this species of malaria does not cause relapse.
Good to know: Plasmodium knowlesi is often misdiagnosed under the microscope as Plasmodium malariae. However, it can be more serious, sometimes causing malignant malaria, and has a relatively high risk of mortality.[9]
Diagnosis
As there are no symptoms that are specific to the disease, it is important that a person see a doctor and mention the possibility of malaria if they experience fever within a year of visiting an affected area.
Other infections may present with similar symptoms, such as typhoid, HIV, dengue fever, meningitis/encephalitis, or viral hemorrhagic fevers, in which blood vessels rupture. Most missed malarial infections are wrongly diagnosed as nonspecific viral infections, influenza, gastroenteritis or hepatitis. Try the Adoctor conditions and symptoms for a free symptom assessment.
A doctor will typically review the person’s medical history and ask about recent travel to tropical climates. A physical exam will also be performed to determine if the spleen or liver is enlarged.
A blood test may be done to confirm the diagnosis. After examination in a laboratory, blood samples can generally show:
- If malaria is present
- What type of malaria is present
- If the infection is caused by a variation of the parasite that is resistant to certain types of drugs
- If the infection has caused anemia
- If the infection has affected any vital organs
Accurate diagnosis of malaria presence and the type of Plasmodium infection is important:
- To ensure appropriate treatment for the best outcome
- Due to concerns of increasing drug resistance, which is widespread in malaria-endemic areas
Sometimes malaria does not show up immediately in a blood test. This happens especially in pregnant people, where the parasite can be present in high numbers in the placenta, without being apparent in the rest of the body.[10] If no malaria is seen in the blood sample, another blood test may be taken a couple of days later.
Treatment
It may be possible to treat malaria at home if symptoms are mild. However, if the infection is caused by Plasmodium falciparum or there are any complications, the person will generally need to be treated and monitored in a hospital.
If promptly diagnosed and treated, most people will make a full recovery from malaria. However, treatment may make a person feel weak and tired for several weeks after the infection is gone.
There are various types of antimalarial medication available. Which medication is prescribed to treat malaria will depend on:
- The subtype of plasmodium parasite causing it
- Whether any antimalarial medications have been taken when traveling
- The severity of symptoms
More than one type of medication, or an alternative, may be given if a person experiences side effects, or if the infecting parasite shows resistance to a particular drug.
Many of the same medications used to prevent malaria can also be used to treat the disease. However, if you’ve taken a particular malaria pill to prevent malaria, you shouldn’t take the same one to treat it.
Certain types of malaria, such as Plasmodium vivax and Plasmodium ovale, have stages in the malaria life cycle where the parasite can live dormant in the liver for several months, even years, and reactivate later, causing a relapse of malaria. If found to have one of these types of malaria, a person will usually be given medication to prevent relapse.
It is possible to be given emergency treatment to take along if traveling to remote places and use it to treat suspected malaria until medical care is available.
Prevention
Malaria prophylaxis is the preventive treatment of malaria. The main ways to prevent malaria are through taking malaria pills, known as chemoprophylaxis, and avoidance of mosquito bites.
There is currently no malaria vaccine available, though development efforts for several malaria vaccines are ongoing.
The World Health Organisation (WHO) recommends five principles, known as the ABCDE of malaria prophylaxis:[11]
- Awareness. When travelling to a malaria-affected area, be aware of the risk of malaria, the malaria incubation period, the possibility of delayed onset and the main symptoms.
- Bite prevention. Use an effective mosquito repellent, such as diethyltoluamide (DEET), and mosquito nets when sleeping.
- Chemoprophylaxis. Take antimalarial drugs when appropriate, starting at least two weeks before entering a malarious area and following the drug’s daily or weekly dosing interval.
- Diagnosis. Seek immediate diagnosis and treatment if a fever develops one week or more after entering an area where there is a malaria risk and up to three months or even later, after departure from a risk area, although symptoms rarely occur after more than three months.
- Environments. Avoid being in or near mosquito breeding areas, such as swamps or marshy areas, particularly in late evenings and at night.
Most frequently, travelers develop malaria because they have not taken their antimalarial medication correctly, either because some doses may have been missed, or the tablets were not taken for the advised length of time before entering or after leaving a malaria-affected area.
Malaria prophylaxis drugs are usually well-tolerated but can result in side effects in some people. The most common side-effects experienced include nausea and diarrhea. Some antimalarial drugs can increase sun sensitivity, making it important to use a higher factor sunscreen, while others might lead to sleep problems and headaches.
Antimalarial medication is not always 100 percent effective, which is why it is important to practice bite prevention when in a malaria-endemic area. Diethyltoluamide (DEET) is the most effective insect repellent, and if the product contains between 10 to 30% DEET it can be used on babies and children over two months of age, and when breastfeeding.[12]. Concerning adults, higher concentrations of DEET may have a longer repellent effect. However, concentrations over 50% provide no added protection.[13]
Other behaviors that will reduce the risk of a person being bitten include:
Using mosquito nets while sleeping, especially those treated with insecticide ensures that there are no holes.
Covering up any bare skin if outside after sunset.
Sleeping in an air-conditioned room, as the lowered temperature discourages mosquitoes.
Putting screens on doors, windows, and other possible mosquito entry routes.
Spraying the bedroom with an insecticide before sleep to kill any mosquitoes that may have entered during the day.
Using an electrically-heated device to vaporize a tablet containing pyrethroid insecticide in the room at night.
Good to know: Herbal and homeopathic remedies have not been shown to be effective for malaria prevention or treatment and are not recommended.
FAQs
Is malaria contagious?
Is there a malaria vaccine?
Can a person acquire immunity to malaria through exposure?
Is malaria caused by a virus or bacteria?
-
CDC. “Malaria.” 26 January 2018. Accessed 28 March 2018. ↩
-
WHO. “Malaria.” Accessed 2 April 2018. ↩
-
CDC. “Malaria – About Malaria.” 13 July 2017. Accessed 30 March 2018. ↩
-
CDC. “Malaria – About Malaria – FAQs.” 20 December 2017. Accessed 4 April 2018. ↩
-
Patient.info. “Malaria.” Accessed 2 April 2018. ↩
-
Malaria.com. “Abdominal Pain in Malaria.” 24 October. 2012 Accessed 3 April 2018. ↩
-
PLOS. “Probability of Transmission of Malaria from Mosquito to Human.” 12 January 2017. Accessed 3 April 2018. ↩
-
Medscape. “Malaria.” 19 September 2017. Accessed 27 April 2018. ↩
-
NCBI. “Plasmodium knowlesi: the emerging zoonotic malaria parasite.” 23 Oct. 2012. Accessed 29 March 2018. ↩
-
NCBI. “Diagnosis of Placental Malaria.” Accessed 30 March 2018. ↩
-
WHO. “Malaria.” Accessed 29 March 2018. ↩
-
NCDHS. “Safe Use of Insect Repellents.” 17 June 2016. Accessed 27 April 2018. ↩
-
CDC. “DEET (factsheet).” Accessed 27 April 2018. ↩
[/trp_language]
[trp_language language=”ar”][wp_show_posts id=”7886″][/trp_language]
[trp_language language=”fr_FR”][wp_show_posts id=”7885″][/trp_language]
**What is Malaria?**
**Malaria** is a life-threatening parasitic disease that is transmitted by mosquitoes infected with the malaria parasite. It primarily affects people in tropical and subtropical regions of the world, particularly in Africa, Asia, and Latin America.
**Transmission:**
Malaria is transmitted through the bite of an infected female Anopheles mosquito. When the mosquito bites a person, the parasite enters the bloodstream through the mosquito’s saliva.
**Symptoms:**
Symptoms may appear within 10 days to 4 weeks after the bite. Initial symptoms include:
* Fever, chills, and sweating
* Muscle pain
* Fatigue
* Headache
If left untreated, malaria can lead to severe complications, including:
* Anemia
* Cerebral malaria (infection of the brain)
* Kidney failure
* Liver failure
**Diagnosis:**
Diagnosis of malaria requires a blood test to detect the parasite. Diagnosis should be prompt to prevent severe complications.
**Treatment:**
Treatment for malaria involves antimalarial drugs, which are prescribed depending on the species of parasite and the severity of the infection. Early treatment is crucial to prevent life-threatening complications.
**Prevention:**
Preventing malaria includes:
* **Using mosquito repellents:** Apply repellents containing DEET, picaridin, or IR3535.
* **Wearing protective clothing:** Wear long sleeves, pants, and socks when mosquitoes are active.
* **Using mosquito nets:** Sleep under insecticide-treated mosquito nets.
* **Antimalarial medication:** In areas where malaria is common, travelers can take antimalarial medication as a preventive measure.
**Impact:**
Malaria is a major public health concern, particularly in vulnerable populations such as children and pregnant women. According to the World Health Organization (WHO), there were an estimated 241 million cases of malaria in 2020, resulting in over 627,000 deaths.
**Keywords:**
* Malaria
* Malaria parasite
* Mosquito-borne disease
* Transmission
* Symptoms
* Diagnosis
* Treatment
* Prevention
* Mosquito repellents
* Mosquito nets
* Antimalarial medication
* Public health concern





Malaria is a terrible disease and researches are still ongoing