What is Chronic Pelvic Pain?
Chronic pelvic pain, or chronic pelvic pain syndrome, is a long-term condition characterized by abdominal pain in the area below the belly button. To be classed as chronic, the pain must be present for at least six months and be severe enough to require treatment or cause functional disability.[1] Chronic pelvic pain can affect men but is most common in women. This resource, therefore, will primarily focus on the condition in women.[2]
There are many possible causes for pelvic pain, including underlying medical conditions such as pelvic inflammatory disease and irritable bowel syndrome, as well as nervous system dysfunction.[1] The condition is also associated with social and psychological factors, including physical and mental abuse.[3] Often, when there is no obvious cause, diagnosis can be difficult, leading to a delay in treatment which can lead many people with chronic pelvic pain to feel dissatisfied or frustrated.
This resource will focus on the condition in women.
Symptoms of chronic pelvic pain
The most typical symptom of chronic pelvic pain is pain in the area below the belly button, which must last for a period of at least six months to be considered chronic.
The specific characteristics and location of the pain typically differ from person to person. Some women describe the pain as constant, while others see it come and go, sometimes triggered by menstrual periods or activities such as eating or heavy lifting. The pain may be stabbing in sensation and focus on a specific area, or it may be dull and spread out over a wider area.
In many cases, the severity of the pain is enough to cause significant distress and interfere with normal activities, such as going to work, exercise, and sexual activity.[4] How the pain feels and when it occurs are often helpful factors in identifying the cause of the pain.
Other possible symptoms of chronic pelvic pain include:
- Abdominal tenderness
- Pain or difficulty while urinating
- A feeling following urination that the bladder has not been completely emptied
- Waking frequently during the night with the need to urinate
- Pain or difficulty during sexual intercourse
- Pain during menstruation, normally accompanied by abdominal cramps
- Headaches
Other symptoms related to the underlying cause of the pain may also occur in some people.
People experiencing possible symptoms of chronic pelvic pain should consult a doctor.
Causes of chronic pelvic pain
The pelvis is the lowest portion of the abdomen, containing a number of organs and complex layers of muscles, nerves and blood vessels. The pain associated with the condition can originate from any part of the pelvis.
The reasons why some people develop chronic pelvic pain are not well understood. However, a number of conditions affecting the reproductive organs, digestive tract, urinary system, muscles and nerves have been associated with chronic pelvic pain. In some cases, psychological factors may also play a role.[1][5]
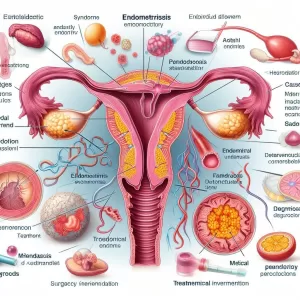
Gynecologic causes
It is estimated that 20 percent of women experience chronic pelvic pain as a result of an underlying condition or problem linked to the reproductive system. Possible gynecologic causes include:[1]
- Endometriosis
- Uterine fibroids
- Adenomyosis
- Pelvic inflammatory disease
- Pelvic adhesive disease
While pregnancy may cause pelvic pain that lasts for over six months, this is not classed as chronic pelvic pain by medical professionals. Due to difficulties in defining the disorder, some doctors also exclude endometriosis as a cause of chronic pelvic pain.
Good to know: Endometriosis is often cyclic in nature, while CPP is not generally considered to be cyclic.
Other causes of chronic pelvic pain
Other, non-gynecologic causes of chronic pelvic pain include:
- Irritable bowel syndrome
- Painful bladder syndrome and interstitial cystitis
- Diverticulitis
- Pelvic pain dysfunction
- Abdominal myofascial pain
- Fibromyalgia
Psychological causes of chronic pelvic pain
In some cases, psychological problems may contribute to the onset of chronic pelvic pain. Moreover, it is thought that the psychological stress that can often result from chronic pelvic pain may help to perpetuate the condition.
Possible psychological factors associated with chronic pelvic pain include:[2][3][5]
- Physical, mental or sexual abuse
- Depression
- Anxiety
Diagnosing chronic pelvic pain
Due to the high number of possible causes of the condition, it can often be difficult to identify the exact source of the pain. A doctor will typically first inquire about the affected person’s symptoms, their medical history and carry out a physical examination. At this stage, the affected person may be required to fill out a symptom questionnaire, as well as undergo a single digit or bimanual vaginal examination.
If there is no obvious cause of the condition after the initial stage of diagnosis, a number of diagnostic tests will typically be carried out.[2]
These tests may include:[1][6]
- Laboratory tests: Such as a blood test, e.g. a white blood cell count, and a urine test.
- Pelvic ultrasound: In which sound waves are used to examine the organs and structure of the pelvic region.
- Pelvic MRI: Magnets and radio waves are used to create an image of the pelvis.
- Pelvic laparoscopy: A procedure involving the insertion of a small, wand-like instrument containing a camera into the pelvis, allowing doctors to view its interior. Although usually considered routine, this procedure does pose risks to the affected woman.
In some cases, tests may not be able to identify the cause of pelvic pain. Although this can make treatment more difficult, it does not rule out treatment altogether. In situations such as these, treatment will be focused on managing the symptoms rather than treating the underlying cause.
Chronic pelvic pain treatment
There is no single way of treating chronic pelvic pain. Treatment will be tailored to the individual and depend on the underlying cause of the condition, its severity and its frequency, and will often involve a number of different methods.
Medication
Pain relief medication will often be recommended to those affected by chronic pelvic pain. At first, over-the-counter medications, including ibuprofen, paracetamol, and aspirin, may be effective. Later, stronger prescription medications may be prescribed by a doctor. Some women may benefit from use of antidepressants. [7]
Physical therapy
Physical therapy can help manage the pain in some cases. Methods include the use of hot and cold applications, stretching and positioning techniques, massage, nerve stimulation and pelvic floor training.[7][8]
Surgery
Some causes of pelvic pain may respond well to surgical treatment. This may involve the removal of the endometrium, a hysterectomy to remove the uterus or a presacral neurectomy, a procedure to remove a group of nerves responsible for sending pain signals from the uterus to the brain.[1]
There is no guarantee that surgery will be effective, and it is usually only considered if the condition has not responded to any other treatment methods.
Counseling
Some women may find that counseling is effective in helping to manage the symptoms of chronic pelvic pain. This may involve one-on-one psychotherapy with a trained psychologist, psychiatrist or social worker, group therapy with other people affected by the same or a similar condition or online or local support groups. Relaxation techniques and biofeedback, a method by which people can learn to control bodily processes that were previously believed to be involuntary or out of their control, may also be effective in some cases.[1]
Chronic pelvic pain prognosis
Typically, chronic pelvic pain can be effectively managed, but not completely cured. In many cases, the condition may go into remission for a period before once again returning, making long-term treatment necessary.
In people who have undergone surgery to manage the condition, pain may still recur, owing to other, undiagnosed sources of pain. Pain may also occur in other areas, such as the lower back or legs, owing to a predisposition to the excessive perception of pain in some people.
Chronic pelvic pain FAQs
u003cstrongu003eCan men experience chronic pelvic pain?u003c/strongu003e
Yes, men can experience chronic pelvic pain. In men, the condition is known as chronic prostatitis/chronic pelvic pain syndrome (CPPS). The key symptom is pain in the pelvic area, usually centered around the penis, scrotum, and perineum. Generally, the pain must be experienced for at least three months to be diagnosed as chronic.u003cbru003eu003cbru003eThe cause of the condition is not yet fully understood. Nerve problems, prostate infection, and autoimmune problems have all been suggested as causes, but there is no medical consensus on the issue. Because of this, treatment can be difficult, and most men will be required to consult a specialist.u003csupu003eu003ca href=u0022https://adoctor.org/wp-admin/post.php?post=4774u0026amp;action=edit#fn9u0022u003e[9]u003c/au003eu003c/supu003e
-
UpToDate. “Patient education: Chronic pelvic pain in women (Beyond the Basics).” December 8, 2017. Accessed December 14, 2018. ↩ ↩ ↩ ↩ ↩ ↩ ↩
-
Patient. “Pelvic Pain in Women.” November 23, 2017. Accessed December 14, 2018. ↩ ↩ ↩
-
BMJ. “Chronic pelvic pain in women.” October 5, 2010. Accessed December 17, 2018. ↩ ↩
-
NIH. “What are the symptoms of pelvic pain?” January 31, 2017. Accessed December 17, 2018. ↩
-
NCBI. “Psychological Factors in Chronic Pelvic Pain in Women: Relevance and Application of the Fear-Avoidance Model of Pain.” October, 2011. Accessed December 17, 2018. ↩ ↩
-
NIH. “How is pelvic pain diagnosed?” January 31, 2017. Accessed December 17, 2018. ↩
-
Medscape. “Chronic Pelvic Pain in Women Treatment & Management.” February 28, 2018. Accessed December 17, 2018. ↩ ↩
-
NIH. “How is pelvic pain treated?” January 31, 2017. Accessed December 17, 2018. ↩
-
Patient. “Chronic Prostatitis.” June 21, 2018. Accessed December 17, 2018. ↩
**Question: What is Chronic Pelvic Pain?**
**Answer:**
Chronic Pelvic Pain (CPP) is a persistent pain in the lower abdomen and pelvic region that persists for at least six months. It affects a large number of individuals, primarily women.
**Symptoms:**
* Pelvic pain that lasts longer than six months
* Pain ranging from mild to severe
* Localized or diffuse pain in the lower abdomen, pelvis, or groin
* Pain associated with menstruation, intercourse, ovulation, or bowel movements
* Other symptoms include fatigue, urinary frequency, constipation, and nausea
**Causes:**
The exact cause of CPP is often difficult to determine. Contributing factors may include:
* Endometriosis
* Interstitial cystitis
* Uterine fibroids
* Pelvic inflammatory disease (PID)
* Irritable bowel syndrome (IBS)
* Nerve damage or entrapment
* Previous surgeries or infections
**Diagnosis:**
Diagnosing CPP involves a comprehensive history, physical examination, and diagnostic tests such as:
* Pelvic exams
* Imaging tests (ultrasound, MRI, CT scan)
* Laparoscopy
**Treatment:**
Management of CPP focuses on identifying and treating the underlying cause when possible. Treatment options may include:
* Medications (painkillers, anti-inflammatories, muscle relaxants)
* Physical therapy
* Pelvic floor exercises
* Lifestyle modifications (e.g., avoiding caffeine, alcohol)
* Surgery (in some cases)
**Complications:**
If left untreated, CPP can significantly impact an individual’s physical, emotional, and social well-being. Complications may include:
* Decreased quality of life
* Sexual dysfunction
* Infertility
* Depression and anxiety
**Prevention:**
While not all cases of CPP are preventable, reducing risk factors may help:
* Managing endometriosis or other underlying conditions
* Maintaining a healthy weight
* Exercising regularly
* Practicing safe sex
* Limiting caffeine and alcohol intake
**Conclusion:**
Chronic Pelvic Pain is a debilitating condition that affects many individuals. By understanding the symptoms, causes, and treatment options, people can seek appropriate medical care and improve their quality of life. If you experience persistent pelvic pain, it is essential to consult a healthcare professional for diagnosis and personalized treatment.
2 Comments
Leave a Reply
Popular Articles







Chronic Pelvic Pain is a condition that affects many women, but is often poorly understood. It can be caused by a variety of factors, including endometriosis, pelvic inflammatory disease, and uterine fibroids.
Chronic Pelvic Pain is a condition characterized by ongoing pain in the lower abdomen and pelvic area.