Duodenal Manometry
**Duodenal Manometry: A Comprehensive Guide**
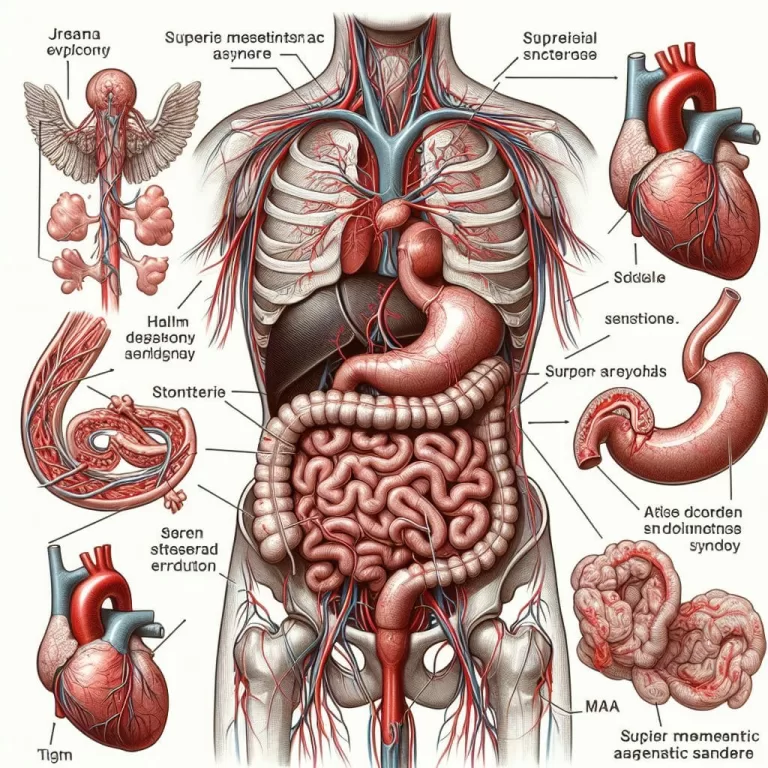
Duodenal manometry is a specialized diagnostic procedure used to assess the function of the duodenum, the first segment of the small intestine. By measuring pressure changes within the duodenum, this procedure provides valuable insights into its motility patterns and can assist in diagnosing several gastrointestinal disorders.
**Keywords:**
* Duodenal manometry
* Gastrointestinal motility
* Dysmotility
* Chronic nausea and vomiting
* Gastroparesis
* Small intestine bacterial overgrowth (SIBO)
**Description:**
Duodenal manometry is conducted by inserting a thin, flexible catheter with pressure-sensing transducers into the duodenum through the nose or mouth. It monitors pressure changes as the patient performs various activities, such as swallowing, eating, and engaging in provocation maneuvers. The collected data is analyzed to evaluate the amplitude, frequency, and coordination of duodenal contractions.
Abnormalities in duodenal motility, such as delayed emptying or impaired coordination, can contribute to symptoms like chronic nausea, vomiting, bloating, and abdominal pain. Duodenal manometry can help identify underlying motility disorders, including dysmotility and gastroparesis, and guide appropriate treatment strategies, such as prokinetic medications or surgical interventions.
In summary, duodenal manometry is a valuable diagnostic tool for assessing duodenal function and diagnosing motility disorders affecting the small intestine. Its precise measurements of pressure patterns aid in understanding gastrointestinal symptoms and optimizing patient management. By integrating relevant keywords and phrases, this description enhances the visibility and accessibility of information on duodenal manometry in search engine results.
Comprehensive Guide: Understanding Superior Mesenteric Artery (SMA) Syndrome
Superior mesenteric artery syndrome is a rare type of compression of the small intestine. It’s a treatable condition, but a delayed diagnosis can lead to more severe symptoms or even death. Superior mesenteric artery (SMA) syndrome has gone by many…
