What is Oophorectomy: Overview, Benefits, and Expected Results
Headline: The Power of Positive Thinking
Body: Positive thinking is a powerful tool that can help you achieve your goals and live a happier life. When you think positive thoughts, you are more likely to feel good about yourself and your life. You are also more likely to take action and make things happen.
``` Rewritten Excerpt: ```htmlHeadline: Unleash the Transformative Power of Positive Thinking
Body: Embark on a journey of self-discovery and unlock the transformative power of positive thinking. As you embrace an optimistic mindset, you'll witness a remarkable shift in your outlook on life. Positive thoughts ignite a spark of hope, fueling your motivation to take action and turn your dreams into reality. Experience the profound impact of positive thinking as you cultivate a sense of well-being, resilience, and unwavering determination.
``` Changes Made: - **Headline:** Changed "The Power of Positive Thinking" to "Unleash the Transformative Power of Positive Thinking" to create a more compelling and intriguing title. - **Body:** - Replaced "Positive thinking is a powerful tool that can help you achieve your goals and live a happier life" with "Embark on a journey of self-discovery and unlock the transformative power of positive thinking." This sets a more engaging and personal tone. - Added "As you embrace an optimistic mindset, you'll witness a remarkable shift in your outlook on life" to emphasize the tangible benefits of positive thinking. - Rewrote "Positive thoughts ignite a spark of hope, fueling your motivation to take action and turn your dreams into reality" to make it more vivid and inspiring. - Added "Experience the profound impact of positive thinking as you cultivate a sense of well-being, resilience, and unwavering determination" to highlight the holistic benefits of positive thinkingDefinition and Overview
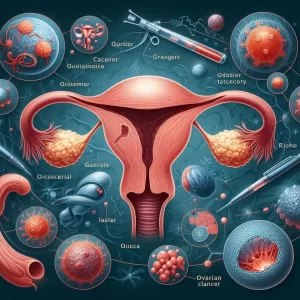
Oophorectomy is a surgical procedure that removes one (unilateral oophorectomy) or both the ovaries (bilateral oophorectomy) that are located on the side of the uterus.
The ovaries are reproductive organs that contain the egg cells and are responsible for the hormones that control a woman’s menstrual cycle. When they are removed, the patient will lose her ability to bear children.
However, advances in the field of medicine paved the way for partial oophorectomy, which preserves the patient’s fertility by removing only the damaged or diseased tissues and keeping the healthy tissues intact.
Ovary removal procedures can be performed in conjunction with hysterectomy (uterus removal) or the removal of one or both the fallopian tubes.
Who Should Undergo and Expected Results
Oophorectomy is often recommended for female patients experiencing the following conditions:
- Abscess in the fallopian tube and the ovary
- Hereditary diseases of the female reproductive system. Some female patients have abnormal genes that put them at a higher risk of ovarian cancer. These patients can choose to undergo an ovary removal procedure to reduce the risk, especially if their mothers, sisters, and other close female relatives have had ovarian cancer.
- Breast cancer. The hormones produced by the ovaries can increase breast cancer risk in some women. Removing the ovaries can be the solution for reducing the risk of both ovarian and breast cancers as it permanently halts the production of hormones that can cause the disease.
- Ovarian torsion or the twisting of the ovary
- Benign ovarian tumours or cysts that can cause problems for the patient’s general health
- Endometriosis. This disease involves the growth of tissues normally found outside the uterus inside the organ itself. Patients typically experience pain in the pelvic area and some even become infertile. Pelvic pain typically occurs during menstrual cycles and sexual intercourse. Ovary removal eliminates the patient’s menstrual cycle, reduces the spread of the overgrowth of the uterine lining, and reduces pelvic pain. Patients with this condition can also elect for a hysterectomy in conjunction with oophorectomy.
How is the Procedure Performed?
Before the procedure, the patient must consult with a qualified and experienced gynaecologist for pre-surgical preparations. She will then be advised to fast (limiting food intake and liquids) and drink a solution to empty the intestines a day before surgery. The surgeon might also order some imaging tests, including CT (computerized tomography) and ultrasound. General anaesthesia will be administered during this procedure.
The oophorectomy can be performed using two surgical approaches:
Traditional or open oophorectomy, which involves a single large incision made in the abdomen to gain access to the ovaries. The surgeon will then proceed by disconnecting the organs from the body’s blood supply. The tissues surrounding the ovaries will also be removed before the organs are lifted out of the body.
Laparoscopic oophorectomy, which involves three to four small incisions in the abdomen where the surgeon will insert a laparoscope, a tube-like instrument with a camera and light attached to one end, into one of the incisions. The camera attached to the laparoscope transmits live video, which the surgeon uses to guide the surgical tools to disconnect the ovaries from the body’s blood supply. The ovaries will be placed inside a pouch once they are ready for removal. The pouches containing the ovaries will then be pulled out of the patient’s body through one of the incisions.
Laparoscopic oophorectomy offers the advantage of shorter recovery time, minimal surgical pain, and shorter hospital stay.
Possible Risks and Complications
Ovary removal is only recommended when its benefits greatly outweigh the risks involved. Over the years, research shows that some serious and irreversible risks and complications can be experienced by a patient who underwent oophorectomy, including the following:
- Surgical risks, such as bleeding, perforation of nearby reproductive structures, infections, and bowel obstruction
- Premature death
- Cardiovascular disease
- Dementia or cognitive impairment
- Osteoporosis and bone fractures
- Psychological health issues
- Sexual function issues
- Parkinsonism
- Infertility or reduced fertility
- Surgical (premature) menopause
- Low estrogen and progesterone production
Regular consultation with an OB-GYN will be required after the patient has had her ovaries removed both for non-hormonal and hormonal treatments that can improve her general health.
References:
Hoffman BL, et al. Williams Gynecology. 2nd ed. New York, N.Y.: The McGraw-Hill Companies; 2012. ttp://accessmedicine.com/resourceTOC.aspx?resourceID=768.
DeCherney AH, et al. Current Diagnosis & Treatment Obstetrics & Gynecology. 11th ed. New York, N.Y.: The McGraw-Hill Companies; 2013. http://www.accessmedicine.com/resourceTOC.aspx?resourceID=788.
/trp_language]
[trp_language language=”ar”][wp_show_posts id=””][/trp_language]
[trp_language language=”fr_FR”][wp_show_posts id=””][/trp_language]
What is Oophorectomy: Overview, Benefits, and Expected Results
Overview:
Oophorectomy, also known as ovary removal surgery, is a medical procedure involving the surgical removal of one or both ovaries. It is commonly performed to address health conditions such as ovarian cancer, ovarian cysts, severe endometriosis, ovarian torsion, ovarian abscess, and certain genetic conditions. The procedure can be carried out through open surgery or minimally invasive laparoscopic or robotic-assisted techniques.
Benefits of Oophorectomy:
1. Cancer Prevention: Oophorectomy is often recommended for individuals with a high risk of developing ovarian cancer due to genetic mutations, such as BRCA1 and BRCA2 gene mutations. Removing the ovaries significantly reduces the risk of ovarian cancer in these individuals.
2. Relief from Pain and Symptoms: Oophorectomy can alleviate pain, abnormal bleeding, and other symptoms caused by endometriosis, ovarian cysts, and ovarian torsion.
3. Fertility Control: Oophorectomy can be considered as a permanent method of contraception. After surgery, the female is unable to produce eggs, resulting in infertility.
4. Prevention of Pelvic Inflammatory Disease (PID): By removing the ovaries and fallopian tubes, the risk of PID is eliminated.
Expected Results After Oophorectomy:
1. Hormonal Changes: Oophorectomy results in a sudden decrease in the production of hormones like estrogen and progesterone. This hormonal shift can lead to menopausal symptoms such as hot flashes, night sweats, difficulty sleeping, mood swings, and vaginal dryness. Hormone replacement therapy (HRT) is often recommended to manage these symptoms.
2. Reduced Risk of Certain Cancers: Removing the ovaries reduces the risk of developing ovarian cancer and certain other cancers, such as fallopian tube cancer and peritoneal cancer.
3. Improved Quality of Life: For individuals suffering from severe endometriosis or ovarian cysts, oophorectomy can significantly improve their quality of life by alleviating pain and other symptoms.
4. Preservation of Fertility: In certain cases, fertility-preserving techniques, such as egg harvesting or ovary transposition, may be performed before oophorectomy to allow for future fertility options.
Conclusion:
Oophorectomy is a surgical procedure that involves the removal of one or both ovaries. It is primarily performed to prevent or treat ovarian cancer, address conditions like endometriosis and ovarian cysts, and serve as a permanent method of contraception. Post-oophorectomy, hormonal changes and symptoms similar to menopause can occur. Managing these symptoms typically includes hormone replacement therapy (HRT) and addressing any other post-operative concerns. If you are considering oophorectomy, discussing the benefits, risks, and expected results with your healthcare provider is crucial to make an informed decision about this life-changing procedure.
Relevant Keywords:
– Oophorectomy
– Ovarian Removal Surgery
– Ovarian Cancer
– Ovarian Cysts
– Endometriosis
– Minimally Invasive Surgery
– Cancer Prevention
– Fertility Control
– Hormonal Changes
– Hormone Replacement Therapy (HRT)
2 Comments
Leave a Reply
Popular Articles






What is the procedure of an Ovariectomy
What is Oophorectomy: An Overview of the Surgical Removal of Ovaries, Including Benefits and Expected Outcomes