What is Rectovaginal Fistula: Symptoms, Causes, Diagnosis, and Treatment?
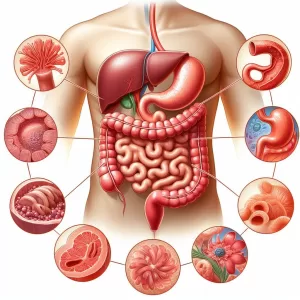
A rectovaginal fistula is a type of fistula that affects the area between the anus and the vagina. It is an uncommon medical condition, although not unheard of in patients who have had complicated childbirths or undergone surgery to treat Crohn’s disease.
What Are the Symptoms of Rectovaginal Fistula?
The most common symptom of a rectovaginal fistula is drainage from the vagina. This drainage is foul-smelling and may contain pus. Other symptoms include:
What Are the Causes of Rectovaginal Fistula?
The most common cause of rectovaginal fistula is trauma to the affected area during childbirth. Other causes include:
How Is Rectovaginal Fistula Diagnosed?
If your doctor suspects you have a rectovaginal fistula, they’ll examine your vagina and anus. They may use a small mirror and light to get a better view of the area.
Your doctor may also perform a sphincterotomy or vaginoscopy to get a closer look at the fistula. During a sphincterotomy, your doctor will make an incision in the affected area to look for signs of a fistula. During a vaginosis your doctor use a speculum to get a better view.
Your doctor may also order an anorectal manometry test or anal electromyography. These tests measure the pressure your muscles generate when you strain or contract them.
Your doctor may also use imaging tests such as MRI, ultrasound, or CT scans to get a better look at the affected area.
Treatment for Rectovaginal Fistulas
Treatment for rectovaginal fistulas depends on the size and severity of the fistula.
Non-surgical Treatment
Surgical Treatment
Surgery is the only permanent solution for rectovaginal fistulas. The type of surgery that’s right for you will depend on the type and severity of your fistula.
Fistulotomy
During a fistulotomy, your surgeon will open up the fistula to try and close it. This is the most common type of surgery for rectovaginal fistulas. However, it may not be suitable if your fistula is too complex or too close to the sphincter muscles.
Advancement Flap Procedures
Your surgeon may also use a flap procedure to repair the fistula. During a flap procedure, your surgeon will move healthy tissue from one area of the body to cover the fistula. This tissue is called a flap.
Perineoplasty
If your rectovaginal fistula is due to trauma from childbirth, your doctor may suggest a perineoplasty. During this procedure, your surgeon will reconstruct the area between the anus and vagina.
Recovery and Outlook
The recovery timeline depends on the type of surgery that was used to treat the fistula and the severity of the fistula.
Your doctor will be able to give you a better idea of the recovery time based on your individual situation. Generally, however, you can expect to have some soreness or discomfort in the area for several weeks after surgery.
The success rate of surgery for rectovaginal fistulas is usually very good. After surgery, the fistula should be completely healed and you should be able to go back to all of your normal activities.
Définition et aperçu
UN fistule is an abnormal tract that forms a tunnel between two organs in the body. If it connects the rectum and the vagina, it is referred to as rectovaginal fistula. Other fistulas that involve the vagina include vesicovaginal fistula (opens into the voies urinaires), colovaginal fistula (opens into the colon), and enterovaginal fistula (opens into the small bowel).
Rectovaginal fistulas, just like other vaginal fistulas, are usually painless and do not represent a life-threatening emergency. However, they can cause significant discomfort and emotional distress as they allow the bowel content and gas to pass through the vagina. This leads to incontinence et les problèmes d'hygiène, qui peuvent avoir un impact sur l'intimité et l'estime de soi.
Causes de la condition
Les fistules rectovaginales se développent généralement à la suite d'un traumatisme lors de l'accouchement. Ils sont souvent observés dans les pays en développement où les soins de santé sont insuffisants. Dans ces pays, les fistules rectovaginales sont l'une des principales causes de décès maternels.
La condition, qui est extrêmement rare dans la culture occidentale, peut également être le résultat d'une épisiotomie, une incision chirurgicale entre le vagin et l'anus pratiquée par une sage-femme ou des obstétriciens lors de l'accouchement pour agrandir l'ouverture vaginale. Cela est souvent nécessaire s'il existe un risque de détresse fœtale grave due à un travail prolongé.
D'autres causes de fistule recto-vaginale moins courantes comprennent :
Principaux symptômes
Les symptômes de la fistule rectovaginale, qui provoquent une gêne physique et une détresse émotionnelle, comprennent :
Qui voir et types de traitements disponibles
Doctors often diagnose the condition during a physical examination and assessment of symptoms of rectovaginal fistula. However, additional diagnostic tests are performed to accurately assess its extent. These tests include:
Bien que les fistules rectovaginales soient faciles à diagnostiquer, elles sont souvent difficiles à guérir et il faut de la patience pendant le processus d'évaluation pour évaluer pleinement l'étendue de la maladie.
Après avoir diagnostiqué une fistule recto-vaginale chez une patiente, il est courant que les patientes subissent une antibiothérapie pendant trois mois maximum pour le traitement de toute inflammation ou infection. Dans certains cas, cela suffit pour que certaines fistules se referment d'elles-mêmes. Cependant, la plupart nécessitent une intervention chirurgicale, qui consiste à inciser la fistule pour qu'elle puisse guérir. Cela peut être fait par le vagin ou le rectum (pour les fistules basses) ou par une incision dans l'abdomen (pour les fistules hautes situées au cul-de-sac postérieur).
During a rectovaginal fistula repair, a sharp circumferential dissection is made to separate the vagina from the rectum. The entire fistulous tract and the small rim of the mucosa are then incised before the rectal wall is closed with incisions.
Le traitement de la fistule rectovaginale consiste également à prélever une greffe de tissu à partir d'autres parties du corps ou à replier un lambeau de tissu sain près de la fistule pour couvrir l'ouverture. Les chirurgiens réparent également les muscles du sphincter anal s'ils ont été endommagés.
Colostomie, a surgical procedure in which feces is diverted to a bag outside of the body to allow the rectum to heal, is also performed in recurrent or complex cases. This is done when there’s scarring caused by previous radiation treatment or surgery, tissue damage, cancerous tumours, significant fecal contamination, or abscess. If a colostomy is performed, treatment of rectovaginal fistula will take place as soon as the rectum has healed, which can take between eight and twelve weeks. After rectovaginal fistula surgery, the colostomy is reversed to restore normal bowel function.
En attendant la réparation d'une fistule recto-vaginale, il est conseillé aux patientes de pratiquer une bonne hygiène pour prévenir l'infection. On leur donne également des antibiotiques et des médicaments pour traiter l'inflammation.
Absolutely, Here’s the FAQ for rectovaginal fistula (RVF)
What is a Rectovaginal Fistula (RVF)?
A rectovaginal fistula is an abnormal connection between your rectum and vagina. This connection allows stool and gas to leak from the rectum into the vagina.
What are the symptoms of RVF?
- Passage of gas, stool, or pus from the vagina
- Pertes vaginales nauséabondes
- Frequent urinary tract infections (UTIs) or vaginal infections
- Pain or irritation in the vaginal area
- Pain during intercourse
What causes RVF?
- Childbirth complications (most common cause)
- Anal or rectal surgery
- Crohn’s disease or other inflammatory bowel diseases (IBD)
- Infections du rectum ou de l'anus
- Traumatisme physique
- Radiation therapy for cervical cancer
How is RVF diagnosed?
- Examen physique
- Anorectal ultrasound
- Blood and urine tests
- Imaging tests (X-ray, CT scan, MRI)
How is RVF treated?
- Antibiotics (for infection)
- Bowel management strategies
- Surgery (the most common treatment):
- Fistulotomy (incising the fistula for healing)
- Flap procedures (using healthy tissue to cover the opening)
- Perineoplasty (reconstructing the area between vagina and anus)
- Colostomy (temporary): for complex cases
What is the outlook for RVF?
Surgery is often successful in closing the fistula. With proper treatment, most women can return to normal activities.
Additional points to consider include:
- Risk factors for RVF (e.g., prolonged labor, instrumental delivery)
- importance of early diagnosis and treatment
- emotional impact of RVF and support resources
Les références:





This is an excellent resource! #knowledgeispower
Good to know – thanks for sharing!
Indeed! #knowledgeiskey